Private Practice Survey Results

Our thanks to the many respondents who provided feedback in our private practice survey run late in 2022. Your input is most valuable towards assisting the NZSA and the Private Practice Network to better identify where we can provide further support for our members working in private practice.
Below we share with you a summary of the survey results.
158 respondents throughout New Zealand completed the survey. Of these 129 work across a mixture of private and public and 22 exclusively in private practice. Most respondents work predominantly in public healthcare, private practice making up one-quarter to one-half of their overall work (Fig.1) and the majority ‘could not choose a preference’ as to which area (private vs public) they prefer to work in (Fig.2). A common theme amongst comments is that each, private and public, has its own positive and negative aspects. Preferences for working in private included predictability, efficiencies, flexibility and remuneration as well as concerns over the current working conditions in the public system. Preferences for working in public focus on the collegiality, collaboration, variety, and professional challenge that can come with the complex cases that arise in the public system.
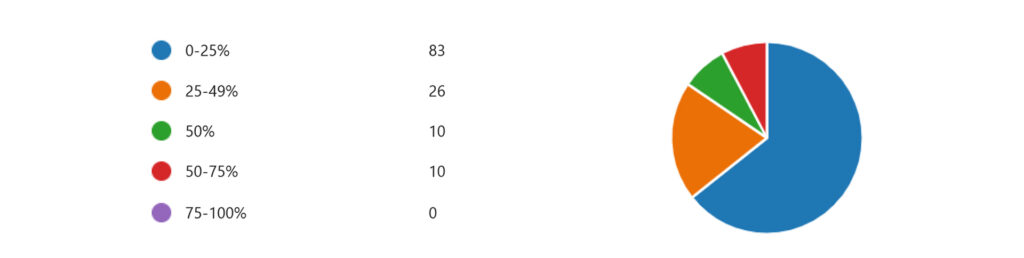
Figure 1. What percentage of your work is in private practice?
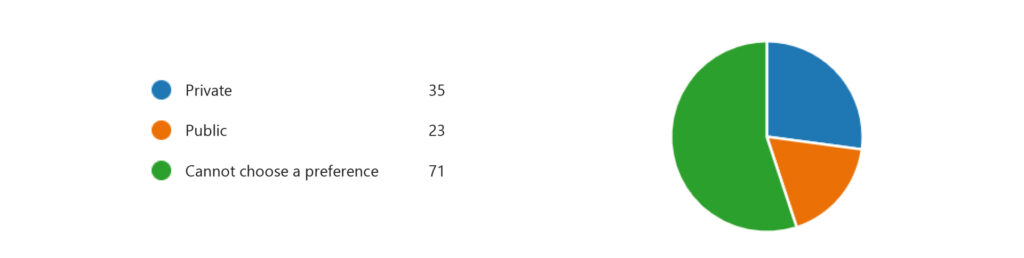
Figure 2. Which do you prefer? (To work in private or public)
Private Practice Facilities
Feedback demonstrates that most private facilities employ anaesthetic technicians or both anaesthetic technicians and nurse assistants to the anaesthetist. The assistant to the anaesthetist is exclusively available to 94% of respondents. The majority are happy with the anaesthesia assistance available to them (Fig.3). Throughout the survey comments note concerns for current staffing shortages and working conditions for assistants to the anaesthetist, an area the NZSA is working to advocate for whenever possible.
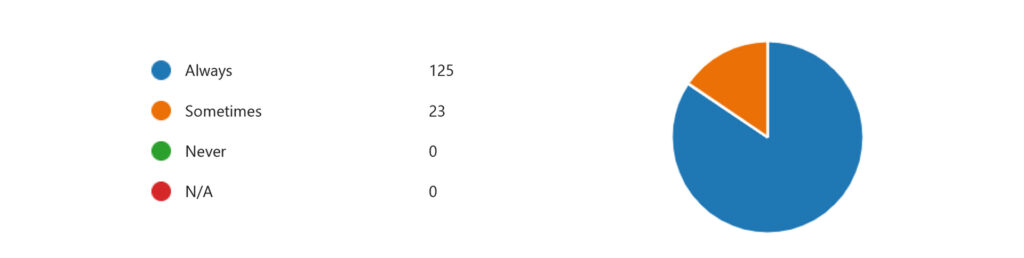
Figure 3. Are you satisfied with the anaesthesia assistance available to you?
Assistance & Equipment
The majority of respondents ‘always’ have access to adequate assistance and equipment to manage difficult airways (82%), MH (78%) and Anaphylaxis (88%). When responding to major bleeds 56% of respondents ‘always’ and 36% ‘sometimes’ have access to adequate assistance. Comments acknowledge there is generally less exposure to these emergencies in private practice.
Most private facilities that respondents are working in do not have onsite RMO cover (13% ‘sometimes’, 79% ‘never’) or daytime anaesthetist cover (96% ‘never’). High care units such as ICUs or equivalent are more varied across the country: ‘always’ available for 22%, ‘sometimes’ for 46%, and ‘never’ for 29% of respondents’ facilities.
Satisfactory pre-assessment set-up is ‘sometimes’ available for most (61%) and always for 29%. Pre-assessment was another theme that arose throughout comments discussing both the varying level each individual offers as part of their service and the varying levels of access to patient information.
The process for transferring patients to a higher care facility or public hospital is ‘sometimes’ and ‘always’ satisfactory for most (Fig.4). The average length of time anticipated for the majority of respondents to be able to start a transfusion when an unexpected bleed occurs is approximately 30 minutes (Fig.5). Additional feedback notes many facilities have O negative blood available on site to be able to begin transfusion.

Figure 4. Is the process of transferring patients to a higher care facility or public hospital (should the need arise) satisfactory?
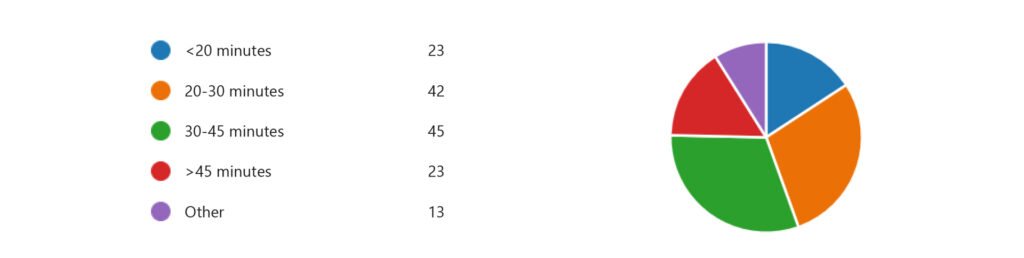
Figure 5. In unexpected major bleeding, on average, how long might it realistically take to transfuse your patient?
Contracts & Billing
ACC
Familiarity with ACC’s clinical services contract (CSC) and elective services contract (ESC) is varied with slightly more familiarity with CSCs than ESCs. Feedback indicates respondents have mixed feelings about ACC reimbursements depending on the procedure (Fig.6) and the majority of respondents (87%) apply modifying units when applicable (Fig.7).
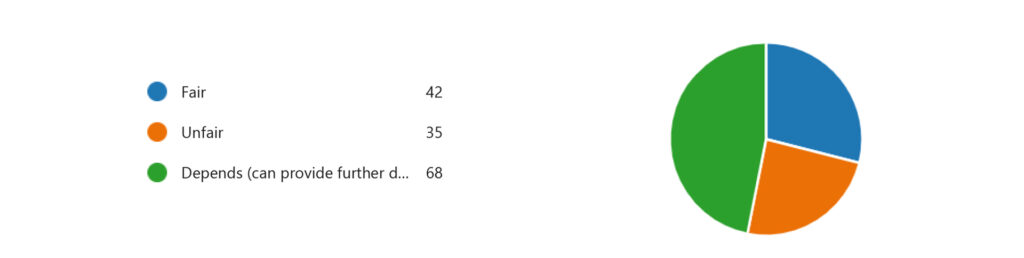
Figure 6. Do you find the amounts reimbursed for procedures
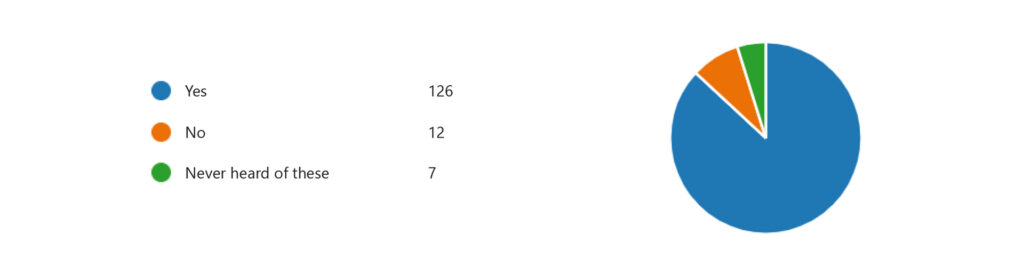
Figure 7. Do you apply modifying units when applicable?
Comments on ACC contracts highlight concerns around inconsistencies, a lack of recognition for the potential complexities of some procedures and some general feelings of being undervalued. This feedback will be most useful to discuss with ACC in our next meeting as examples of the challenges we are facing and to be able to establish areas we can work together to make improvements.
Southern Cross
There is much more familiarity with Southern Cross contracts in comparison to ACC contracts. However, the same as ACC contracts, the adequacy in remuneration for most APS contract procedures for the majority of respondents, depends on the procedure. 49% of respondents feel they would charge ‘generally more’ if not under an APS contract and 40% would charge ‘about the same’. Reflection on adequate recognition in APS contracts for pre-op assessments, intra-op complexity, unusually long cases and post-op care is greatly varied among respondents (Fig. 8).
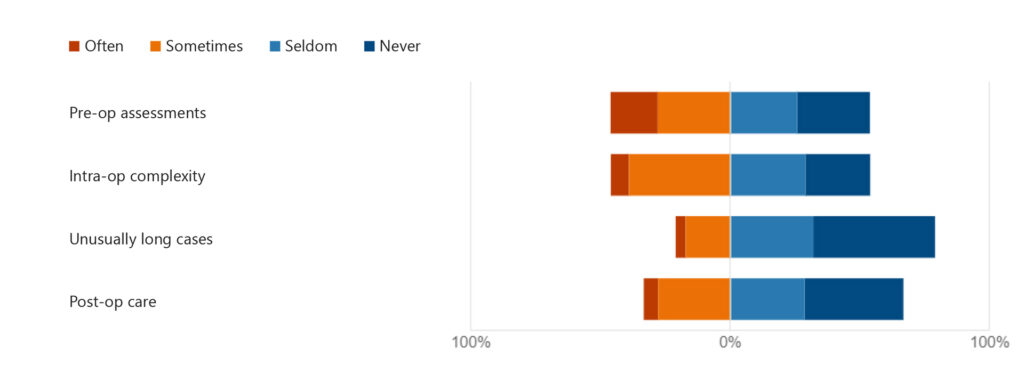
Figure 8. Do APS contracts adequately charge for
Themes within comments in the ‘Southern Cross’ section highlight concerns with current Southern Cross contracts. A consistent feeling amongst these is that remuneration is calculated on surgical time or complexity with less recognition for the anaesthesia technicalities involved or pre- and post-op consultation and time.
Anecdotal evidence would suggest that private practice anaesthetists are being underpaid in certain circumstances under the Southern Cross APS fixed fee system. The NZSA would like to make a case to Southern Cross Insurance to demonstrate this and obtain their agreement to allow the addition of RVG-based modifier units to the fixed APS fee, when the situation warrants it. There is already a precedent for this with ACC coded procedures. Of course, we need to have a robust case to put forward – and for this, we need evidence. If you would be willing to assist please contact Membership Manager, Deanna Smith at membership@anaesthesia.nz.
We are simply determining who is willing to assist with the provision of information – in principle only at this stage. Once we have determined a group and have a good spread across New Zealand the next step will be to fine-tune the data collection process and ensure all is legally sound. We need to be very mindful of not comparing fees and avoid any discussion about such things as price, fee, unit dollar amount or any other reference to pricing that could be considered as us colluding.
Private Practice Work Satisfaction
Consistent themes amongst comments on current work concerns in private practice include:
- Resourcing and emergency response for some private facilities. Particularly as more public procedures are being outsourced to private, bringing cases with higher complexities to facilities with fewer emergency resources.
- Staffing and assistant to the anaesthetist shortages.
- Disillusionment towards decisions made around private practice contracts and reimbursement that do not fairly recognise anaesthesia service and experience.
- Fair resourcing and recognition across specialties.
- Adequate pre-operative patient information or assessment.
- Billing and pricing processes and clarity.
Whilst unfortunately the NZSA and Private Practice Network cannot help to address everything, identifying the concerns of members across the motu does assist us in recognising opportunities where we can offer the most assistance and best informs future planning.
Key themes that arise in feedback on what respondents enjoy most in their private practice work include:
- Collegiality and working with a consistent and familiar surgical team.
- Better efficiencies.
- Flexibility and predictability of caseloads and lists.
- Patient contact and influence on their procedure and experience.
- A calmer working environment, often noting the catered lunch and coffee, or the break it offers from days working in the public system.
Thoughts on where respondents feel the NZSA can provide further assistance and areas of interest for future educational topics are most helpful. These will be further discussed with planning groups to see where we can incorporate them into future events and the development of resources.


